Georgia Open Enrollment Checklist for 2025-26: A Step-by-Step Guide
Georgia Open Enrollment Checklist for 2025-26: A Step-by-Step Guide
At a Glance: Georgia's open enrollment period for 2025-26 runs from November 1, 2025 through January 15, 2026. For businesses, a successful period requires months of advance planning from September through early December to ensure successful benefits administration, compliance with regulations like COBRA, and the best possible outcomes for both employers and employees.
Open enrollment is one of the most critical periods in the annual benefits administration cycle, requiring careful planning and strategy. Well-planned open enrollment creates opportunities to improve employee satisfaction, ensure regulatory compliance, and position benefits packages as competitive advantages in talent acquisition and retention. However, inadequate preparation can lead to missed cost-saving opportunities, employee confusion, compliance risks, and potential coverage gaps.
Following a month-by-month timeline before, during, and after the open enrollment period can help Georgia employers make sure that nothing falls through the cracks during this critical period.
Key Deadlines for Open Enrollment
Georgia's open enrollment period for the 2025-26 plan year runs from November 1, 2025, through January 15, 2026. This federally mandated timeframe applies to health insurance marketplace plans and typically aligns with employer-sponsored plan enrollment periods.
Missing these enrollment deadlines typically means employees cannot make changes until the next period unless they experience qualifying life events. Late submissions can result in coverage gaps or delayed implementation.
Successful execution requires beginning preparations months earlier, which provides plenty of time for strategic planning, carrier negotiations, and employee education.
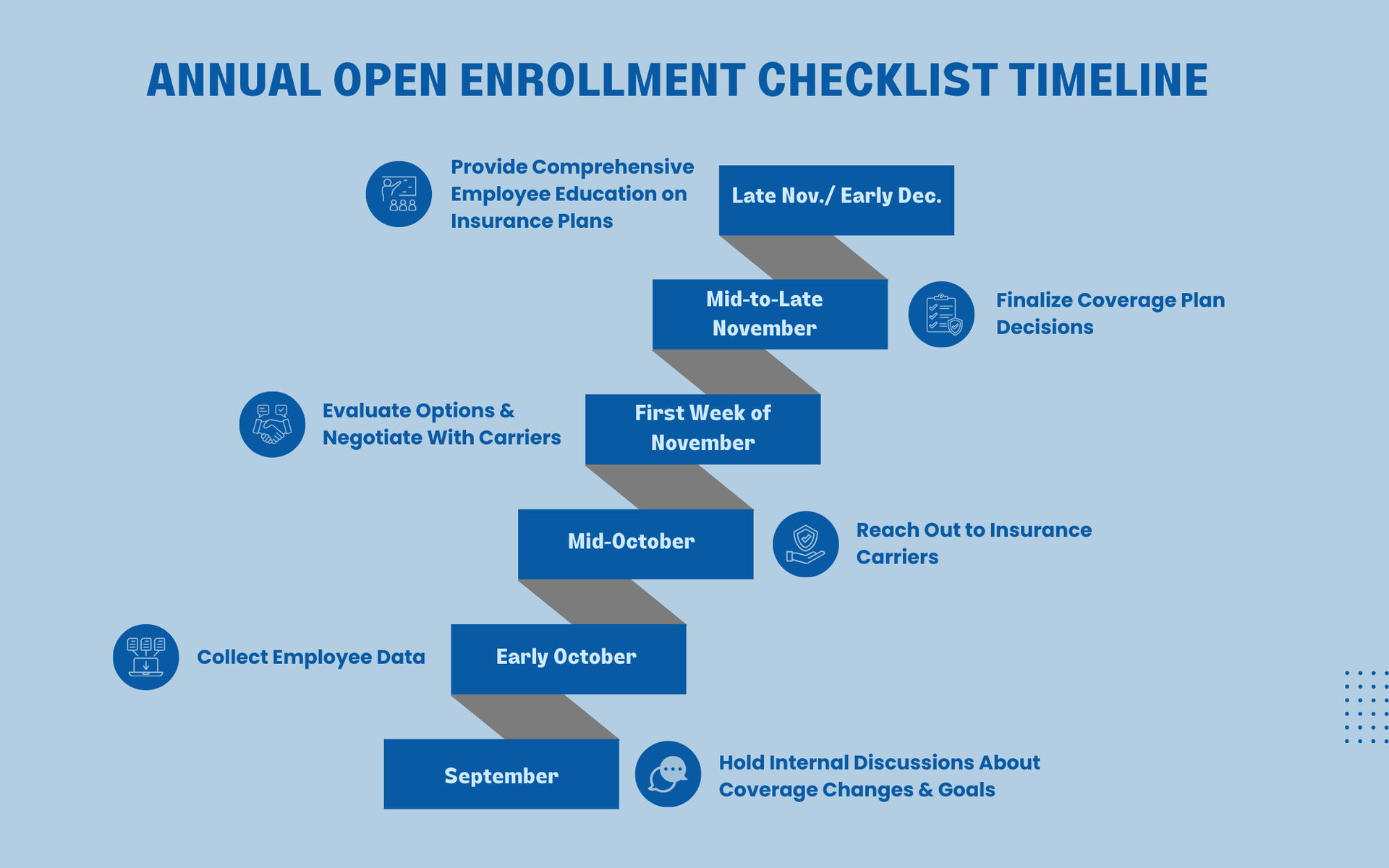
Open Enrollment Timeline
September: Building a Foundation & Strategy Plan
Begin internal discussions about goals and potential changes during September. HR leadership, finance teams, executive decision-makers, and anyone else who provides input on organizational priorities and budgets should be involved in this planning.
Understanding what your employees value can guide strategic decisions about where to invest benefits dollars for maximum impact.
- Consider employee needs through analysis of previous year's feedback surveys, demographic changes, and emerging healthcare trends
- Evaluate your current coverage and how it is affected by budget constraints, financial objectives, or other business priorities
- Explore additions to enhance your group health coverage like vision insurance, dental insurance, Health Savings Accounts (HSA), or Flexible Spending Account (FSA)
Early October: Data Collection
Collect comprehensive employee census data, including:
- Headcounts
- Dependent Information
- Age and Demographic Details
- Salary Information
- Health Needs
- Geographic Distribution
Carrier pricing considers employee age distribution, dependent ratios, geographic locations, and claims history. Providing accurate data is important to ensure appropriate pricing from insurance carriers.
Mid-October: Carrier Engagement and Specialized Considerations
Initiate the formal quotation process by sending your updated information to insurance carriers. This information should include comprehensive census data, current plan details, specific coverage requirements, and budget parameters.
Specialized Considerations
Industry-Specific business insurance plans can address unique risks in your sector. For example, construction companies face different needs than most businesses, requiring specialized coverage options and carriers experienced in the challenges faced in that industry.
Consider engaging benefits consultants or brokers who specialize in your industry and provide valuable insights into best practices, emerging trends, and negotiation strategies that optimize outcomes.
First Week of November: Evaluation and Negotiation Period
Receive and thoroughly evaluate carrier proposals, comparing options across multiple dimensions including premium costs, plan designs, out-of-pocket maximums, and administrative service quality.
Enter negotiation discussions with carriers, leveraging competitive proposals to secure optimal terms. Negotiation opportunities may include premium pricing adjustments, enhanced coverage features, improved administrative support, and wellness program additions.
Don't hesitate to push back on initial proposals. Carriers expect negotiation and often have flexibility, particularly for employers with favorable claims experience or growing employee populations.

Mid-to-Late November: Finalization and Communication Planning
Finalize plan decisions based on a comprehensive evaluation of all benefit offerings, including medical, dental, vision, life insurance, disability coverage, and supplemental benefits. For future reference, document the decisions you made and the reasons you made each of them.
Prepare comprehensive employee communication strategies ensuring workforce members understand their options. Effective communication planning includes developing clear benefit summaries, creating comparison tools, scheduling informational meetings, preparing FAQs, and establishing channels for individual questions.
End of November/Early December: Employee Education and Enrollment
Employers should address all employees with any changes in coverage, explain available options, and answer questions. Open enrollment meetings and presentations should cover all available benefit options, explanation of changes, guidance on evaluating personal needs, enrollment instructions, and opportunities for questions.
Educate employees on the value of their complete benefits package, helping them understand total compensation beyond salary. Some of these methods include-
- Providing total compensation statements showing employer contributions
- Explaining how to maximize healthcare coverage through preventive care
- Demonstrating how to navigate insurance systems effectively.
- Offering multiple enrollment support options (in-person assistance, online resources and tutorials, dedicated helplines, and one-on-one counseling) to ensure that all employees receive appropriate support
Additional Features and Things to Note
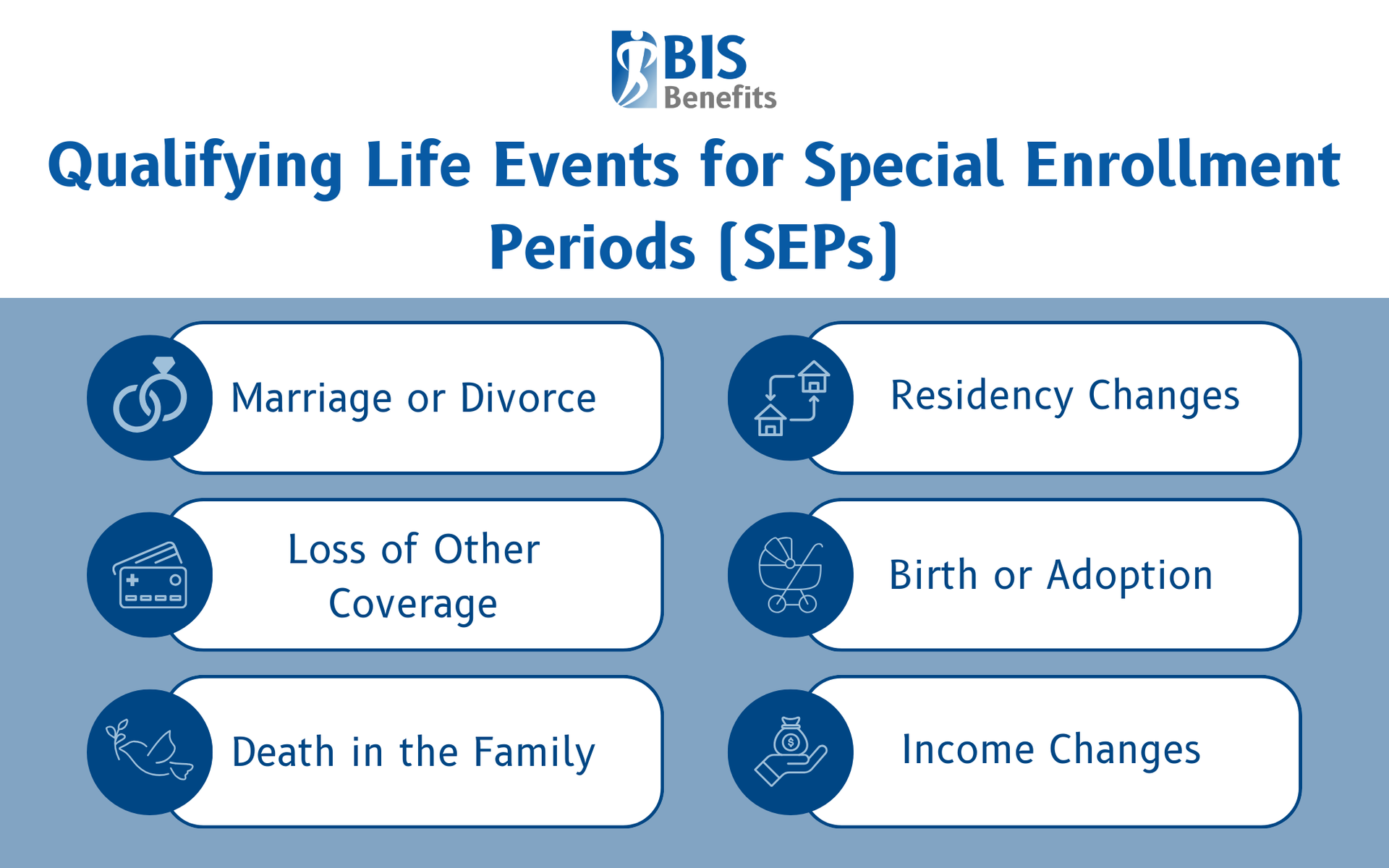
Special Enrollment Periods (SEP) in Georgia
A Special Enrollment Period provides coverage access outside regular open enrollment for individuals experiencing qualifying life events (QLEs). SEPs support workforce flexibility and employee satisfaction during these significant life transitions. Understanding SEPs is particularly important for small businesses managing ongoing workforce changes.
Eligibility requirements for qualifying life events include-
- Marriage or Divorce
- Birth or Adoption
- Loss of Other Coverage
- Changes in Residence
- Income Changes
Employees experiencing these events typically have either60 or 90 days to request special enrollment from
Georgia Access.
COBRA Compliance
Georgia employers with 20 or more eligible employees must comply with COBRA (Consolidated Omnibus Budget Reconciliation Act) regulations, which require offering continued health insurance coverage to employees and their dependents following qualifying events such as termination, reduction in hours, or other life changes.
Employers must provide COBRA election notices within 14 days of a qualifying event and allow eligible individuals 60 days to elect continuation coverage. Non-compliance can result in costly penalties, so it's important for businesses to understand these obligations.
COBRA Administration services can help businesses stay on top of necessary record-keeping, timely notifications, and accurate premium collection.
Benefits Enrollment Software
Modern benefits enrollment software creates opportunities for increased efficiency and accuracy through streamlined processes. Quality platforms offer opportunities, including-
- Employee Self-Service
- Automated Eligibility Verification
- Integration with Payroll Systems
- Comprehensive Reporting Capabilities
- 24/7 Access
Investing in enrollment technology typically generates significant returns through reduced administrative time, fewer enrollment errors, improved employee satisfaction, better data accuracy, and enhanced compliance documentation.
How BIS Benefits Helps You Make the Most of Open Enrollment
Navigating Georgia's open enrollment landscape is a challenge that many businesses struggle to manage effectively. You need a broker who understands this landscape and can guide you through every phase of open enrollment. The certified agents at BIS Benefits specialize in expert group benefits and business insurance services that transform this annual obligation into a strategic opportunity.
BIS Benefits’s comprehensive approach begins with understanding your unique organizational needs, workforce demographics, and budget parameters. We provide strategic guidance on health plans, benefits trends, and workforce management to help you understand what's working with your current plan and where more opportunities are available. We leverage our relationships with all major insurance carriers in Georgia to negotiate competitive rates. Our brokers handle the complex details, freeing your staff to focus on employee education.
Request a Quote from BIS Benefits today to discuss how our expertise can simplify your 2025-26 open enrollment and position your benefits package as a competitive advantage in Georgia's business marketplace.