What Businesses Should Know About COBRA Insurance in Georgia
What Businesses Should Know About COBRA Insurance in Georgia
At a Glance: COBRA is a federal law that allows employees and their dependents to continue group health coverage after a qualifying event like job loss, reduced hours, or divorce. Federal COBRA applies to Georgia employers with 20 or more employees, while smaller employers may be subject to Georgia Mini-COBRA, which provides similar protections but with a shorter coverage period of 90 days.
Losing health insurance coverage can be one of the most stressful parts of a job change or major life event for employees. For businesses, handling that transition incorrectly can also create serious compliance risks. COBRA insurance exists to provide a temporary safety net, allowing employees and their families to continue their group health coverage when it would otherwise end.
For Georgia employers,understanding COBRA is important because both federal COBRA and Georgia’s state continuation laws may apply, depending on your company’s size and health plan structure. Missteps in notice timing, eligibility determinations, or premium handling can expose businesses to penalties, lawsuits, and unexpected liability for medical claims.
What Is COBRA Insurance?
COBRA stands for the Consolidated Omnibus Budget Reconciliation Act, a federal law designed to protect employees and their dependents from sudden loss of health insurance coverage.
COBRA allows individuals who lose coverage due to certain qualifying events to continue the same group health plan they had while employed. COBRA continuation coverage acts as a bridge during periods of transition, such as job loss, reduced work hours, divorce, or other life changes.
Under COBRA:
- Healthcare coverage is identical to the active employee plan
- The employee or beneficiary pays the full cost of monthly premium payments
- Employers may charge up to a 2% administrative fee
- Health benefits are temporary, not permanent
TheUnited States Department of Labor (DOL) administers and enforces COBRA, and it applies to most private-sector and public employers that meet size requirements.
Which Georgia Employers Must Offer COBRA?
Federal COBRA applies to employers with 20 or more employees. This threshold is based on employee counts during the previous calendar year. Georgia employers must consider the following requirements:
- Both full-time and part-time employees count
- Part-time employees count as a fraction of a full-time employee, equal to the number of hours worked divided by the hours a full-time employee must work
- The employer must have met the 20-employee threshold on more than 50% of typical business days in the prior year
- Applies to private-sector employers and state or local government employers
- Does not apply to federal government plans or certain church-related organizations
Businesses with fewer than 20 employees are exempt from federal COBRA, but that does not mean they have no obligations. In Georgia, smaller employers may still be subject to Georgia Mini-COBRA requirements.
Georgia Mini-COBRA Coverage for Small Employers
Georgia’s State Continuation law (Georgia Mini-COBRA) applies to employers with fewer than 20 employees that offer fully insured group health plans. While similar in purpose to federal COBRA, Georgia Mini-COBRA has important differences that small businesses must understand.
Key characteristics of Georgia Mini-COBRA:
- Applies to employers with less than 20 employees
- Applies primarily to fully insured plans, not self-funded plans
- Allows employees to continue coverage after certain qualifying events
- Coverage duration is typically limited to 90 days, much shorter than federal COBRA
- Insurers may not charge the standard 2% administrative fee
Because Georgia Mini-COBRA rules differ from federal COBRA, employers must clearly understand which law applies to their business. Applying the wrong rules can result in compliance violations, even if the intent was correct.
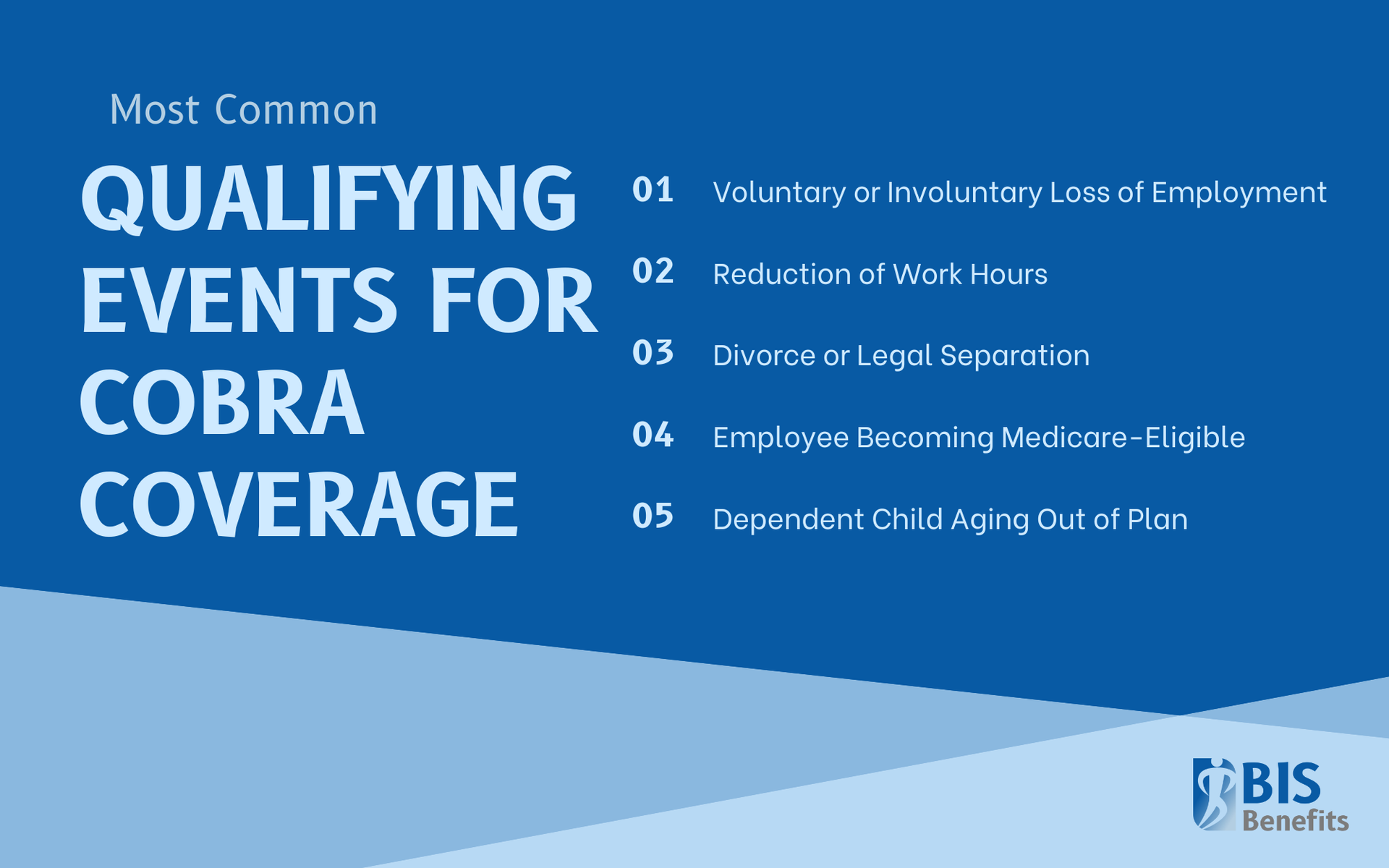
Qualifying Life Events That Trigger COBRA Coverage
COBRA coverage is triggered by specific events that cause a loss of health insurance coverage. Employers are responsible for recognizing these events and responding appropriately.
Common
qualifying events include:
- Voluntary or involuntary termination of employment (apart from gross misconduct)
- Reduction in work hours resulting in loss of healthcare plan coverage
- Death of the covered employee (dependents may qualify)
- Divorce or legal separation from the covered employee
- Employee becoming eligible for Medicare
- Dependent child aging out of plan eligibility
Once a qualifying event occurs, the employer must act quickly to notify the plan administrator and ensure required notices are sent on time.
Who Is Eligible for COBRA Coverage?
COBRA eligibility requirements extend beyond just the employee. Qualified beneficiaries may include:
- Covered employees
- Spouses covered under the group plan
- Dependent children covered under the plan
To be eligible, individuals must have been enrolled in the group health plan the day before the qualifying event occurred:
- Employees terminated for gross misconduct are not eligible
- Dependents may elect COBRA independently, even if the employee declines coverage
Understanding these distinctions is essential to avoiding improper denials or missed notices.
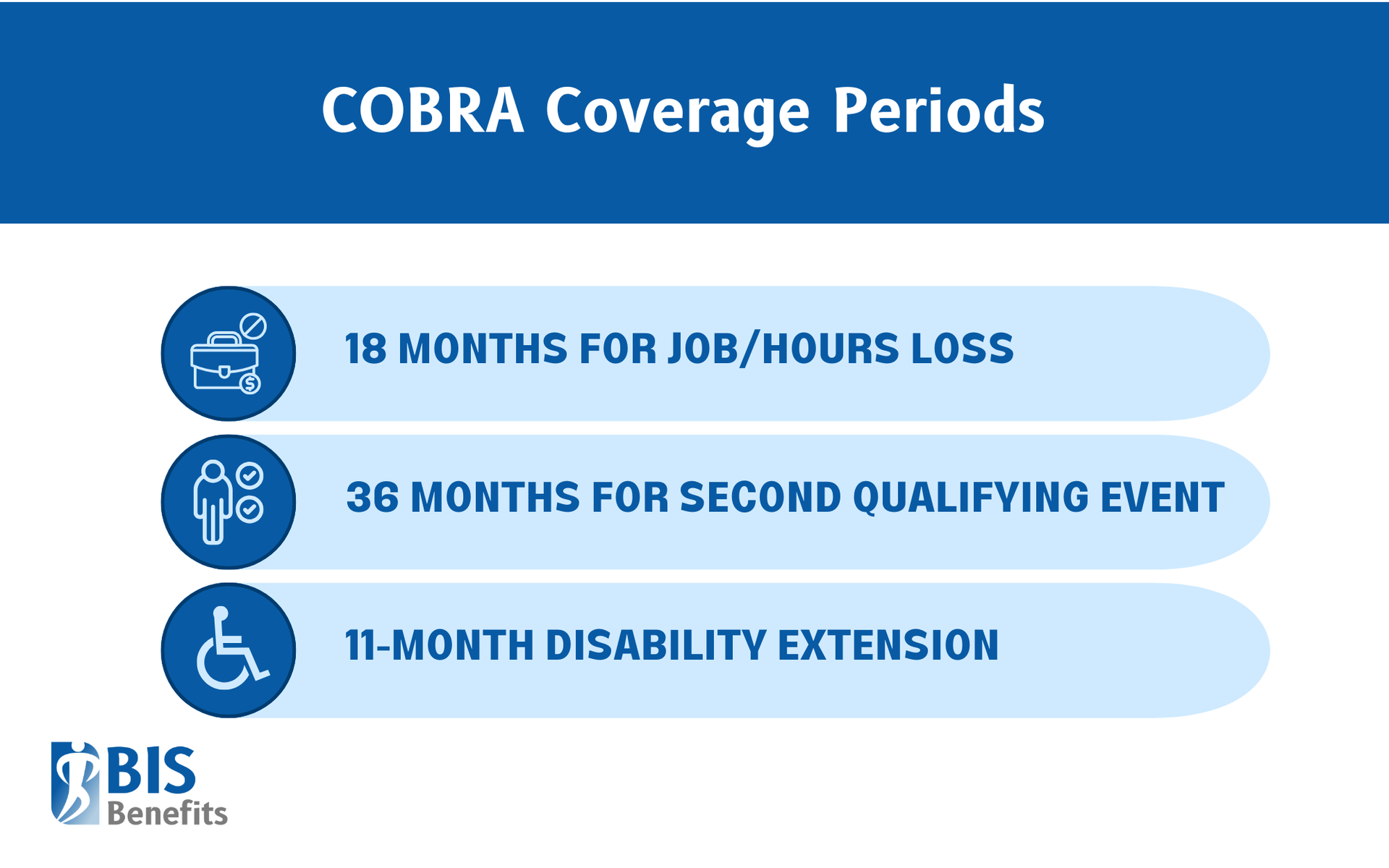
COBRA Coverage Duration
The length of COBRA coverage depends on the type of qualifying event.
Standardcoverage periods include:
- 18 months for job loss or reduction in hours
- 36 months for a second qualifying event affecting dependents, such as death, divorce, Medicare eligibility, or a child aging out
Additional extensions may apply:
- An 11-month disability extension may be available, bringing total coverage to 29 months
COBRA coverage may end early if:
- Premiums are not paid on time
- The employer stops offering a group health plan
- The beneficiary gains coverage under another group plan or Medicare
Employer COBRA Responsibilities and Compliance
Employers play a central role in COBRA compliance. Failure to meet notice and timing requirements is one of the most common causes of violations.
Key
employer responsibilities include:
- Providing an initial COBRA notice when an employee enrolls in the group health plan
- Notifying the plan administrator within 30 days of a qualifying event
- Ensuring an election notice is sent to qualified beneficiaries within 14 days
- Allowing beneficiaries 60 days to elect COBRA coverage
- Maintaining documentation of all notices and communications
- Coordinating with insurance carriers or third-party administrators
Penalties for non-compliance can include:
- IRS excise taxes
- Civil lawsuits
- Court-ordered medical expense reimbursement
- Attorneys’ fees and penalties

COBRA Costs: What Employers and Employees Should Expect
Under federal COBRA, employees may be charged up to 102% of the total premium, which includes:
- The employee portion
- The employer portion
- Up to 2% for administrative costs
If a disability extension applies, premiums may
increase to 150% during the extension period.
While employers are no longer required to subsidize coverage, they must continue offering access to the plan. Because COBRA premiums can be expensive, clear communication is critical so employees understand their options and costs.
Common COBRA Compliance Mistakes to Avoid
Georgia employers frequently run into trouble due to avoidable errors, including:
- Missing required notice deadlines
- Misidentifying qualifying events
- Miscounting employees and misunderstanding which COBRA law applies
- Poor documentation of notices and elections
- Ignoring Georgia Mini-COBRA requirements
- Failing to coordinate with third-party administrators
- Terminating coverage prematurely
Even small administrative mistakes can lead to significant financial exposure.
Best Practices for Georgia Employers
To manage COBRA effectively and reduce risk, Georgia employers should:
- Work with a qualified third-party COBRA administrator
- Train HR staff on qualifying events and notice deadlines
- Track employee counts carefully
- Maintain organized COBRA records
- Review plan documents annually
- Communicate clearly and compassionately with departing employees
Find COBRA Administration Solutions for Your Business with BIS Benefits
Business owners whose companies have 20 or more employees need to be familiar with COBRA coverage. At BIS Benefits, our expert insurance brokers can help you understand the federal requirements for COBRA and the steps you need to take to set your business up for success. Request a Quote from BIS Benefits today to learn more about our COBRA Administration, Group Benefits, and Commercial Insurance services help Georgia businesses.